What Is an Electronic Health Record (EHR)?
An electronic health record is a digital file with an individual’s medical history, including diagnoses, lab results, medications, treatment plans, and allergies. Electronic health records can be easily shared, with permission, between other providers across multiple organizations.

Other types of data an EHR typically includes:
- Conditions or diseases
- Allergic reactions
- Contact information
- Family history
- Immunization status
- Information about any surgeries or procedures performed
- Information about visits to healthcare professionals
- Insurance information
- Medical images
- Patient consultation reports
- Patient demographics
- Records of hospital visits or hospitalization
- Communications with health care professionals
Benefits of EHRs
- Aggregate anonymized patient data and make it available for research
- Comply with regulatory rules
- Enhance patient satisfaction
- Expedite diagnoses
- Improve physician productivity
- Improve security for protected health information
- Keep medical records updated
- Provide 24/7 access to patient information
- Reduce transcription costs
- Save time by digitizing administrative tasks
- Share medical information between different offices and organizations
Key Features of Electronic Health Records
Electronic Health Records for Office Administration
Schedule management allows for optimal scheduling and provides an easy interface to stay on top of it.
Patient status can be tracked, including check-in, room assignments, updates, notifications, and reporting.
Task assignment and prioritization can be managed, including setting the flow of work assignments, delegating tasks, and tracking tasks through completion.
Clinical documentation can be generated, including patient-specific care plans, organizational guidelines, and order entry.
Electronic Health Records to Support Physicians
Patient charts are easily accessible and can be quickly parsed to bring up relevant information.
Recording capabilities allow clinicians to add information to a patient's records in several ways, including completing templates, dictation, or handwriting notes.
Reports generation capabilities allow physicians to quickly create standard patient-specific reports, such as a medication list, clinical notes visits, treatment plans, medical histories, and patient care orders.
ePrescribing records prescriptions in the patient’s record and transmits them directly into the pharmacy’s computer system. The system can also flag any drug interaction warnings at the time of medication order.
Notifications can be sent letting patients know about preventive services, tests, or appointments that are coming up or overdue. The system can also track if actions have been taken and, if not, send follow-up notifications.
Data segmentation allows administrators to tag and share only parts of patients’ electronic health records to ensure privacy.
Electronic Health Records for Patient Portals
Proactively participate in care by reviewing visit activity, tracking symptoms, scheduling a follow-up appointment, getting automated appointment reminders, having a virtual appointment, paying bills online, requesting a prescription refill, or sending messages to providers.
Electronic Health Record Implementation
A multi-disciplinary approach is required for electronic health record implementation.
10 Steps for Successful Electronic Health Record Implementation
- 1. Build an implementation team
Include physicians, nurses, receptionists, medical assistants, compliance staff, and administrative staff. These representatives provide insights into issues and potential challenges.
- 2. Optimize workflows
Before starting the electronic health record implementation, take time to review and optimize workflows so they can be embedded in the new systems. Considerations for optimizing workflows are:
- Is it necessary?
- Does it add value for the patient or the practice?
- Is it being done in the optimal order?
- Is it being done by the right person?
- Does this require the skills and training of a physician or can a staff member do it?
- 3. Consider the space layout
Electronic health records mean that computers, laptops, or tablets must be available to capture information. From the front desk to the exam room, consider where these will be placed to ensure patients’ privacy as well as provide easy accessibility for all users.
For exam rooms, consider how people will be sitting and interacting. When at all possible, the medical team should not be turning their backs on patients to enter data into the electronic health record system.
- 4. Identify hardware needs
Work with the electronic health record implementation vendor to identify the right hardware to support the new systems. This goes beyond servers. Consider who will use the electronic health record system and how it will be used.
For instance, more printers throughout the office could improve productivity. For security purposes, servers may be located in a locked room. The electronic health record vendor and staff members can assist with the hardware need assessment.
- 5. Configure the software
The electronic health record implementation vendor can help with software configuration. To expedite this, identify data that should be integrated into the new system, such as patient history and billing information.
In addition, pay close attention to security. It is imperative that security measures are in place to ensure HIPAA compliance.
- 6. Transfer data
Once hardware and software are in place, data needs to be migrated to the new electronic health record system. Making a checklist of the data to transfer helps ensure that all necessary information is moved to the new system.
Once the data migration is complete, it is recommended that the legacy systems be kept in place for a period of time in case data is overlooked and still needs to be moved. After all data is in the new electronic health record system, work with an IT expert to ensure that all sensitive information on old systems is destroyed.
- 7. Develop a launch plan
When the electronic health record implementation is complete, there are two choices for how to launch—incrementally or all at once. There are merits to both approaches. When evaluating the options, consider the pros and cons of each and the logistics of the rollout.
- 8. Establish procedures for electronic health record system’s downtime
Preparation reduces the impact of unexpected system downtime. Take time to develop a plan for what staff should do in the event that the electronic health record system is not available. It is recommended that hard copies of these instructions be available and to keep a copy in cloud storage as a backup.
- 9. Create a training plan
Train staff and physicians to ensure a successful launch of the electronic health record implementation:
- Start by explaining why the new system was implemented and its benefits.
- Training should be tailored to each user type.
- Materials should be presented and provided in document form for reference later.
- Training should be incremental; start with the basics, then move on to training on the more advanced features for those who need it.
- Create a plan for refreshers and updates on new features or changes to the system.
- 10. Set up a system for collecting feedback
A successful electronic health record implementation requires ongoing optimization. Solicit and use input from users to address issues and make incremental improvements.
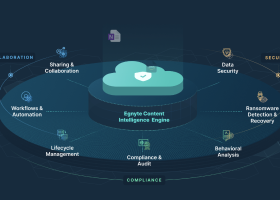
Data Governance, Privacy, and Regulation
Data governance ensures that electronic health records are effectively managed and protected. It also provides healthcare organizations with a standardized and structured method of sharing medical data. HIPAA and HITECH are the two primary laws that protect Americans’ protected health information (PHI), including electronic health records.
Health Insurance Portability and Accountability Act (HIPAA)
HIPAA identifies who is allowed access to medical records and protects PHI. It also ensures the protection of electronic health records during transfer and storage.
The Health Information Technology for Economic and Clinical Health (HITECH) Act
The HITECH Act empowers the Federal Department of Health and Human Services (HHS) to oversee the quality, safety, and security as well as the secure information exchange related to health IT systems, including electronic health records.
Electronic Health Records and Data Breaches
Medical records have become a more sought-after target, because they fetch a higher black market price. The consequences of a data breach can be costly in terms of fines, remediation, and reputation damage.
Data breaches that target electronic health records fall into two categories—those caused by software vulnerabilities and those resulting from human error. Electronic health records can be subjected to a data breach in a number of ways, including phishing, malware, ransomware, or technical vulnerability exploits.
Electronic Health Records for Efficiency and Security
There are many benefits to electronic health records. Security is noted as one of the best.
Despite concerns about electronic health records and data breaches, electronic health records are far more secure with digital protections than in file drawers. Additionally, the overall increase in efficiency cannot be overstated. Physicians and staff agree almost universally that electronic health records save them time and are easier to use and manage than their paper predecessors.
Egnyte has experts ready to answer your questions. For more than a decade, Egnyte has helped more than 16,000 customers with millions of customers worldwide.
Last Updated: 5th December, 2021