Pharmacodynamics
Pharmacodynamics is the qualitative study of what a drug does to the body (i.e., to target cell types, tissues, organs) in terms of biochemical or molecular interactions, as well as how it moves through and out of the body. Pharmacodynamics studies the relationship between drug dosage (i.e., concentration or exposure) and pharmacological or toxicologic responses (i.e., therapy or adverse effects).

Pharmacodynamics follows drug absorption, bioavailability, distribution, metabolism, and excretion to determine the onset, duration, and intensity of a drug's effect. A drug's pharmacodynamics can be affected by a number of physiologic changes related to:
- A disorder or disease
- The aging process
- Other drugs
Uses for Pharmacodynamics Analysis
- Quantify the rate and magnitude of exposure to a drug
- Predict dosage requirements
- Predict the biological effect of changes to dosage requirements
- Estimate the rate of absorption and excretion
- Compare a new formulation's absorption to an existing formulation
- Characterize intra- and inter-subject variability
- Identify variables that affect concentration-effect relationships
- Estimate margin of safety based on the therapeutic index (a ratio that compares the blood concentration at which a drug becomes toxic and the concentration at which the drug is effective)
Pharmacodynamic Mechanisms for Drug Absorption
Pharmacokinetics helps measure a drug's absorption and subsequent bioavailability, or the fraction of administered drug that reaches circulation. Potential routes of administration include the following.
Enteral
Administered orally, this method of drug administration is the most common, convenient, economical, and painless, but also the least predictable. The drug must remain stable until it is absorbed in the gastric environment.
This is inherently unpredictable, because there are many variables that can impact the rate of absorption, such as the pH of the gastrointestinal tract, gastric motility, the presence of food in the stomach, and the patient's adherence to the prescribed drug regimen.
Subcutaneous
Small volumes of oil-based drugs are administered. The subcutaneous route enables a slow rate of drug absorption and maintains steady-state concentrations.
Intramuscular
This route allows for rapid absorption of aqueous solutions, while oil-based formulations provide slow, constant absorption.
Intravenous (IV)
Intravenous administration provides rapid onset of action and allows controlled drug delivery to adjust the dosage based on a patient's response.
Intrathecal
With the intrathecal route, drugs are administered into the fluid-filled space between the layers of tissue that cover the brain and spinal cord. This route bypasses the blood-brain barrier, allowing drugs to reach their target the fastest.
Mucous Membrane
Highly vascular routes of mucous membranes, such as sublingual, ocular, nasal, pulmonary, and rectal, allow for rapid absorption of drugs.
Transdermal
Because drugs are absorbed into the systemic circulation slowly across the skin and subcutaneous tissues, this route is used for drugs that require prolonged administration.
Pharmacodynamic Interactions
Pharmacodynamic drug-drug interactions refer to when the actions of one drug are changed in the presence of another. The result of these interactions is the drugs have either additive effects, which increase the overall effect, or opposing effects, which decrease or even neutralize the overall effect. Pharmacodynamic drug-drug interactions can occur at the level of drug:
- action
- effect
- response
Four Groups of Pharmacodynamic Interactions
There are four main groups of pharmacodynamic interactions that vary and can be exacerbated by genetic differences between individuals.
- 1. Synergistic interactions
The action of an index drug is enhanced by another, which could increase the risk of overdose. - 2. Antagonistic
The main action of a drug is opposed by another, which can reduce the effects of one or both drugs. - 3. Interactions secondary to changes in drug transport mechanisms
For example, the actions of one drug can be blocked. - 4. Interactions due to disturbances in fluid and electrolyte balance
An example is one drug blocking the secretion and excretion of another, which can result in concentrations and subsequent toxicity.
Pharmacodynamics and Drug Actions
Affinity
The most common pharmacodynamic mechanism is the activation of receptors and biological responses. The affinity of the drug is based on how it binds to the receptor. Drug-receptor binding creates complex chemical interactions that deliver the drug.
Dose-Response Relationships
A dose-response relationship associates outcome risk, either increasing or decreasing, with heightened levels of exposure to a drug. The two main types of dose-response relationships are graded and quantal.
The graded dose-response curve shows the effect of various doses or concentrations of a drug as related to potency and efficacy. The quantal dose-response curve demonstrates the average effect of a drug based on its dose, measuring effectiveness, toxicity, and lethality.
Therapeutic Window
A therapeutic window is a range of doses that elicits a therapeutic response without causing any significant adverse effect (i.e., unacceptable toxicity) in patients. It is quantified by the therapeutic index.
Pharmacodynamic Biomarkers
Pharmacodynamic biomarkers are molecular indicators of a drug's effects and are used to understand the correlation between drug regimen, target effect, and biological response. Two categories of pharmacodynamics biomarkers are drug-specific and general.
Drug-specific biomarkers show changes in the biochemical and physiological functions produced by the drugs. General biomarkers reflect nonspecific physical or chemical interactions.
Because they reflect the interaction between a drug and its pharmacological target, pharmacodynamic biomarkers enable precise dose adjustment based on an individual's molecular responsiveness to the therapy. Pharmacodynamic biomarkers also have the potential for enabling the selection of a very specific therapeutic approach for an individual in a number of cases, including therapy with biologics, anticancer, immunosuppressive, antiepileptic, psychotropic, anticoagulant, and procoagulant drugs.
Pharmacodynamics and Therapeutic Drug Monitoring
Therapeutic and drug concentration decisions can be improved with pharmacodynamics by directly measuring the physiological indices of biomarkers, including lipid concentrations, blood glucose, blood pressure, and clotting.
Therapeutic monitoring using pharmacodynamics is valuable when:
- A good correlation exists between the pharmacologic response and plasma concentration, which allows for the prediction of pharmacologic effects with changing plasma drug concentrations
- A dose results in wide variation in plasma drug concentrations across subjects
- Therapeutic concentration is close to the toxic concentration (i.e., has a narrow therapeutic index)
- Desired pharmacologic effects cannot be assessed readily by other simple means (e.g., blood pressure measurement for anti-hypertensives)
Pharmacokinetic characteristics of a drug create variability in the concentration achieved when a given dose is administered to different people. This variability is the result of one or more of the following:
- Variations in drug absorption
- Variations in drug distribution
- Differences in an individual's ability to metabolize and eliminate the drug
- Disease states that impact metabolism and excretion due to compromised liver or kidney function
- Physiologic states (e.g., extremes of age, obesity) that alter drug absorption, distribution, or elimination
- Drug interactions
Pharmacodynamics for Safer More Effective Therapeutics
Most potential drug interactions can be recognized by applying the principles of pharmacodynamics. Quantifying how drugs affect the body with pharmacodynamics ensures safe and effective usage. Because of pharmacodynamics, researchers and clinicians are able to prescribe drugs to achieve optimal outcomes.
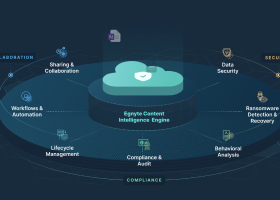
Egnyte has experts ready to answer your questions. For more than a decade, Egnyte has helped more than 16,000 customers with millions of customers worldwide.
Last Updated: 18th December, 2021